Why Compression
 Compression therapy can be used to treat several circulatory issues and improve patient’s overall health. In addition to helping those that suffer symptoms it also provides preventative care which is an important benefit.
Compression therapy can be used to treat several circulatory issues and improve patient’s overall health. In addition to helping those that suffer symptoms it also provides preventative care which is an important benefit.
- Compression stockings help your body pump blood back to your heart is it moves through the legs.
- It can be likened to a tube of toothpaste… When you squeeze the bottom of the tube, the toothpaste migrates up and out. You are applying the most pressure to the very bottom and the pressure is decreasing as it moves up the tube.
Graduated medical compression therapy applies measured amount of pressure to the leg with the most pressure at the ankle and gradually lessening pressure up the leg. The same principle is applied to arm sleeves with the highest pressure at the wrist lessening toward the bicep. This helps the blood in the veins flow back toward your heart, even if your veins and valves are damaged. It is used to manage and help prevent the progression of vein-related diseases.
The use of compression socks are also used to help reduce the severity of muscle soreness and accelerate the recovery of muscle function following strenuous exercise. In the US, compression is expressed in millimeters of mercury (mmHg). The US FDA recognized two medical classes of compression. Medical class 1 stockings are “medical support for general medical purposes” and medical class 2 stockings are “medical support to prevent pooling of blood in legs”. An important distinction is that there is not a correlation between a specific compression level and the claim. It is up to the legal manufacturer or distributor to support their specific claims.
U.S. Standard of Compression
There is not a US standard of compression, but generally accepted practices include:
Mild (8-15 mmHg) Gentle compression and support aiding in the prevention of minor leg and ankle swelling.
Moderate (15-20 mmHg) Moderate compression is great for mild edema, minor varicose veins, good for during and after pregnancy, good for traveling, and considered preventative.
Firm (20-30 mmHg) Firm compression is good during and after pregnancy, after vein procedures, use to treat moderate edema, helps prevent recurring ulcers, and helps protect against DVT.
Extra Firm (30-40 mmHg) Significant compression typically used for active venous ulcers, severe edema, and varicose veins.
Conditions that may benefit from compression therapy
Edema (swelling)
 An abnormal accumulation of fluid trapped beneath the skin very commonly found in the feet and legs
An abnormal accumulation of fluid trapped beneath the skin very commonly found in the feet and legs
Causes: Medications; liver or kidney disease; heart failure; venous insufficiencies; pregnancy/hormones, paralysis, surgery, lymphatic problems
Treatment: Treat the underlying cause, compression hosiery (or arm sleeves), lifestyle modifications, medications, properly fit shoes, and leg elevation.
Spider Veins
 Chronic venous disease occurs when the veins in your legs are not working effectively and it becomes increasingly difficult for blood to pass through the vein walls or valves to flow back to your heart. There are six stages of the disease, from spider veins in the earliest stage to open sores in the most advanced stage.
Chronic venous disease occurs when the veins in your legs are not working effectively and it becomes increasingly difficult for blood to pass through the vein walls or valves to flow back to your heart. There are six stages of the disease, from spider veins in the earliest stage to open sores in the most advanced stage.
In its mildest stage, CVD appears as spider veins, which may look like small red or blue tree branches or spider webs close to the skin surface. Spider veins may then develop into varicose veins, which are enlarged, rope-like blood vessels that are swollen and raised above the surface of the skin. In CVD’s more advanced stages, symptoms such as leg swelling with varicose veins may be present. You may also begin to see skin changes in your legs (usually a darkening of the skin or a rash due to pooling of blood and increased pressure in the veins). Or you may see a sore with a scab, usually on one or both of your inner ankles. In CVD’s most advanced stage, an open ulcer (sore) with oozing fluid may be present. Chronic venous insufficiency (CVI) is another name for the more advanced stages of CVD.
While the progression of chronic venous disease does not appear to be affected by one’s gender, or favor one leg over the other, there are several risk factors:
- Age (over 50)
- Family history of varicose veins
- History of deep vein thrombosis (DVT)
- Obesity
- Smoking
- Pregnancy
- Prolonged periods of standing or sitting
- Damaged or diseased valves
Chronic Venous Insufficiency (CVI)
 Long standing condition where venous pressure fails to decrease with walking. The valves in the deep venous system are damaged or destroyed and veins cannot pump enough blood back to the heart. Progresses if not treated with symptoms including shiny brown weepy skin, itchy, dull discomfort, pain when standing, recurrent ulceration is common.
Long standing condition where venous pressure fails to decrease with walking. The valves in the deep venous system are damaged or destroyed and veins cannot pump enough blood back to the heart. Progresses if not treated with symptoms including shiny brown weepy skin, itchy, dull discomfort, pain when standing, recurrent ulceration is common.
Causes: Family history, pregnancy, diet, trauma/surgery, fracture, obesity, inactivity, age
Treatment: Anticoagulants, bed rest (acute cases), elevate leg, exercise, gradient compression during ambulation
Varicose veins
 Varicose veins affect both men and women.
Varicose veins affect both men and women.
Causes: Back up of blood in the veins caused by hereditary, pregnancy, occupation, or age.
Symptoms: Bulging veins, aching and discomfort in thigh, leg heaviness and fatigue, inflammation
Treatment: Compression hosiery helps relieve symptoms and slow progress; sclerotherapy, laser surgery, endovenous thermal ablation, microphelbectomy, endoscopic perforator vein surgery and other procedures are used.
Pregnancy & Varicose veins

- 30% of women experience varicose veins in their first pregnancy.
- 55% of women experience varicose or spider veins in their second or subsequent pregnancy.
Factors: Hormones, pressure of the fetal head, and 40-50% increases in blood volume.
Treatment: Compression Stockings are beneficial and recommended during pregnancy and post-partum.
Deep Vein Thrombosis (DVT)
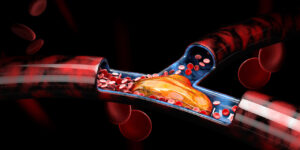 DVT is a blood clot in a deep vein. It is estimated that over 2 million people develop DVT in the US every year with a recurrence rate of approximately 30%. Recurrence rate can be cut in half through compression therapy. Half of DVT patients had no prior symptoms.
DVT is a blood clot in a deep vein. It is estimated that over 2 million people develop DVT in the US every year with a recurrence rate of approximately 30%. Recurrence rate can be cut in half through compression therapy. Half of DVT patients had no prior symptoms.
If a DVT, or part of one, breaks away and gets into the bloodstream, it can block blood flow to the lungs. This is called a pulmonary embolism. A large pulmonary embolism can be deadly. Pulmonary embolism, along with DVT, kill as many as 180,000 Americans each year, more than the number of people who die from breast, prostate, colon, and skin cancers combined. Estimated that 1 in 100 patients that suffer a DVT will die.
Causes: Inactivity, recent surgery, pregnancy, oral birth control pills, hormone replacement therapy, inherited blood clotting disorder, age, prolonged immobility, obesity, long surgical procedures, history of venous disease, and being big & tall.
Treatment: Compression hosiery (both for prevention and treatment) and blood thinners
American College of Clinical Pharmacy (ACCP) guidelines call for compression therapy for a minimum of two years after DVT
Stasis dermatitis
 Inflammatory skin disease usually occurring in the lower extremities, often a precursor to venous ulcers. Presents as darkening of the skin at ankles/legs, itching and flaking, skin appears thin tissue-like or can be hard and scar-like. Estimates that it affects 1 million people per year in the US
Inflammatory skin disease usually occurring in the lower extremities, often a precursor to venous ulcers. Presents as darkening of the skin at ankles/legs, itching and flaking, skin appears thin tissue-like or can be hard and scar-like. Estimates that it affects 1 million people per year in the US
Causes: Fluid accumulation in tissues beneath skin, capillaries unable to remove waste, tissue becomes malnourished and fragile. Other causes include elderly, diabetes, obesity, peripheral vascular disease, smoking, sedentary life-style, varicose veins, or chronic venous insufficiency.
Treatment: Compression, topical steroids, antibiotics, lifestyle modifications, vein surgery
Venous leg ulcers
 Form at the end stage of venous insufficiency; an open wound usually found on inside of ankle, usually with irregular borders, may have partial skin loss, may have yellow or greenish discharge, painful to stand. An estimated 1 – 2 million people in the US suffer from leg ulcers and 30% will experience recurrence without treatment.
Form at the end stage of venous insufficiency; an open wound usually found on inside of ankle, usually with irregular borders, may have partial skin loss, may have yellow or greenish discharge, painful to stand. An estimated 1 – 2 million people in the US suffer from leg ulcers and 30% will experience recurrence without treatment.
Causes: Chronic venous insufficiency, varicose veins, sedentary or non-ambulatory, edema, history of DVT, or a family history of leg ulcers.
Treatment: Compression, Lifestyle modifications, nutrition evaluation, Antibiotics, topical wound care, surgery
Summary of Venous Disorder Symptoms & Warning Signs
- Tired, heavy-feeling legs
- Edema, swollen legs/ankles especially at night
- Varicose/spider veins
- Tingling, numbness, burning or cramping in the legs
- Discoloration of the skin
- Open sores or ulcers on the lower leg
- Family history of vein problems
- Pregnancy
Select claims, rationale for the claim, and peer reviewed reference are available for existing customers. For the best product and application please contact us.
Anatomy & Circulatory System

The main function of arteries, veins, and capillaries is to move blood throughout the body. Blood makes a roundtrip through the body about 1,000 times every day.
Arteries carry oxygen rich blood away from the heart (walls must withstand great internal pressure). Capillaries are the communication point between arteries and veins. Veins carry blood back to the heart.
The venous system can be compared to roadways with deep veins carrying 90% or more of the blood back to the heart. Superficial veins can be compared to local highways and handle 10% or less of the blood flow. Perforators are the on and off ramps. Unlike arteries, veins have valves that keep blood flowing toward the heart.
The calf muscle is often considered the second heart because it plays a role within the circulatory system that is like the heart. One pump of the heart exerts enough power to send blood throughout the body reaching the lower extremities in just seconds. That oxygen-rich blood flows through arteries and capillaries to reach every cell of the body, providing oxygen and nourishment.
The oxygen-depleted blood then needs to travel back up through veins to reach the heart, where it will pass into the lungs to receive a replenishing supply of oxygen. The problem is that traveling back up to the heart takes more force than a single pump of the heart can provide because the blood is flowing counter to gravity. To get the job done efficiently, the veins need negative energy from the pumping heart plus stimulation from what is now known as the “calf muscle pump.”
 USA / English
USA / English Canada
Canada México / Español
México / Español